Interview with a TCCC (Tactical combat casualty care) instructor
29 April 2022Friends, recently we had the opportunity to talk to a real Tactical combat casualty care instructor who came to Ukraine from the United States to teach our Armed Forces soldiers tactical medicine.
 Mike is a certified USCG instructor, paramedic, and military medic. So, we couldn't help but ask Mike some interesting questions about hypothermia and share our mini-interview with you."
Mike is a certified USCG instructor, paramedic, and military medic. So, we couldn't help but ask Mike some interesting questions about hypothermia and share our mini-interview with you."
Hello Mike! It's great that you have the opportunity to give back to Ukraine in this difficult time, thank you for your support!
That's why I'm here! Glory to Ukraine!
Mike, we want to ask you about the relevance of the problem and the physiology of hypothermia, can you say a few words about that? 14pt; line-height: 19.9733px; font-family: "Times New Roman", serif;">So, when the human body begins to cool down, a whole range of phenomena actually occurs.The heart rate decreases, but the blood pressure rises, and this affects certain organs: the heart, blood vessels, and brain.
Elderly people, especially those with medical problems, can have heart attacks, strokes, etc. When the internal temperature drops, every degree makes a difference.
One positive side of hypothermia is that it can slow down the metabolism and oxygen demand of the brain. Usually, if you don't get oxygen to the brain for 6-10 minutes, you dieis. But there is a phenomenon called the "mammalian diving reflex" (mammalian diving reflex), especially if you are immersed in cold water, even a temperature of 6 to 8 degrees can cause irreversible consequences in the brain. That's when compensatory mechanisms kick in to slow everything down: your heart and your brain, and start transferring blood from your extremities to the main system.
This is a response to a situation where, for example, a person is found under the snow and cannot be reached for 30-40 minutes. The victim goes into cardiac arrest. But when the person is finally reached and successfully resuscitated, it is due to the "mammalian diving reflex". This is possible when your core temperature is slowly dropping, but these are rare cases. It usually happens when you are suddenly immersed in water or a cold environment.
Unfortunately, when you are already bleeding, for example, from a gunshot wound or for another reason, hypothermia has a critical effect. Just a drop in internal temperature of a few degrees causes what we call "coagulopathy", which makes it even more difficult to coagulate your blood.
That's why, the loss of just a litre of blood causes the following symptoms.So, you can lose about a litre of blood, which is already enough to cause symptoms. And if you are hypothermic at the same time, it's as if you have lost two litres of blood. And you can die because of your body's inability to clot."
That is why we attach such an important role to the issue of warming patients in TCCC (Treatment of Casualties in Combat Casualty Care). In TCCC and MARCH protocol: massive bleeding, airway obstruction cause shock. And intravenous infusions and hypothermia are related.
If you start intravenous infusions and the solutions are cold, you worsen the patient's condition. You need to make sure that the intravenous solutions are warm. Therefore, we use the heat of the human body itself (we put them near the human body), use chemical heaters, etc.
In the MARCH protocol, the letter "H" stands for hypothermia and head injury, and that's why we pay so much attention to it. Obviously, if the internal temperature drops and you put the wounded person in a vehicle that does not have a heater inside, like an ambulance, then you should try your best to warm the patient and maintain the temperature (especially if they are bleeding)."
I think your question was about hospital intensive care, right?
And about her too.
For example, if people fall off a pier (or something similar), they can drown in cold water. They don't take a lot of water into their lungs, but when they are pulled out, they don't breathe normally, or they don't breathe at all, or they can sometimes go into cardiac arrest, especially if they are elderly. Therefore, our hospitals have only in the last few years launched programmes (scenarios) that can be used to properly warm a patient who has a mammalian diving reflex. Doctors also transfuse warm blood and make sure that everything is warm. And we do not warm the periphery! We don't cover the patient with blankets, especially the arms and legs (!), because such actions cause a rush of blood to these areas, and we want all the blood to be in your heart, brain and kidneys, the main organs. I'm not a "hospital guy", I'm in the field all the time, so I'm not sure what the exact mechanism is, but I do know that you should only go to hospitals that know how to warm a hypothermic person properly.
So, as I understand you, you heat infusion solutions even in the field where a person has been injured? 14pt; line-height: 19.9733px; font-family: "Times New Roman", serif;">Only if you are sure that the solution is warm, you should infuse. If the solution you need is just sitting in the ambulance and the temperature is between 0° and 10°, and you know it, you need to warm it up before you give it to the patient because you will cause them even more hypothermia if it is cold.
So there are different ways (I mean, in the field), the best way is to put the IV solution next to the body. But you shouldn't give cold IV solution anywhere.
We have devices called space heaters and air heaters, and you've probably heard of them. I'm guessing, because I know you even have ultrasound in ambulances here, and our ambulances in San Diego don't. You know, we have EKGs, pulse oximeters, capnographs, we have all of that, but we don't have a really good ultrasound machine like you have: 16pt; line-height: 22.8267px; font-family: "Times New Roman", serif;">At each stage of care, does the infusion solution need to be heated? 14pt; line-height: 19.9733px; font-family: "Times New Roman", serif;">Yes. To the best of my knowledge.
It sounds primitive and easy, but we must remember this at every period: hospital, pre-hospital. Sometimes doctors forget about it, unfortunately.
Yeah, exactly! I mean, if you have those warmers, they're a big help with the IV solution. You can even start the IV solution while it's warming up, but don't give the patient all the solution until it's warm.
And speaking of ultrasound, what do you think, is the device useful in an ambulance? Is it really necessary?"
I think so. I don't have a lot of experience from attending conferences where they demonstrate different ultrasound machines that allow you to see blood flow and the abdominal cavity. That would be valuable, and to be honest, it's been a few years since I've been to one of these conferences where they demonstrate ultrasound machines. If I had this device, I would use it all the time.
You know, this is one of those things that requires skills and qualifications. But you guys, I mean here [in Ukraine], you can use ultrasound for many purposes.
Have you seen ultrasounds in ambulances?
Yes, we even have our own ultrasound sensors, portable ones that can work with phones or computers or laptops, that's very useful I think.
Yes!
But, in fact, not many ambulances in Ukraine have ultrasound: 14pt; line-height: 19.9733px; font-family: "Times New Roman", serif;">Well, I guess it's just the doctors in the ER, right?
When I was here eight years ago, I saw them. 8 years ago, you had ultrasound in ambulances, but we still don't have that practice in the United States. Well, if you have that, especially with abdominal treatment... You know, the difference between diagnosing and treating abdominal is a complicated issue, it could be the liver, it could be the pancreas, it could be anything, it could be bleeding in the abdomen, it could be a lot of things where people have abdominal pain in one part or another. And it's difficult to make a diagnosis unless you have the tools to look at the abdominal cavity. And ultrasound is exactly one of them."
Good, thank you for your opinion, for the opportunity to talk about hypothermia and even about ultrasound.
Of course, Okay!
Thank you! Thank you!
Slava Ukrainie!
Heavy Hail to the Heroes!
-
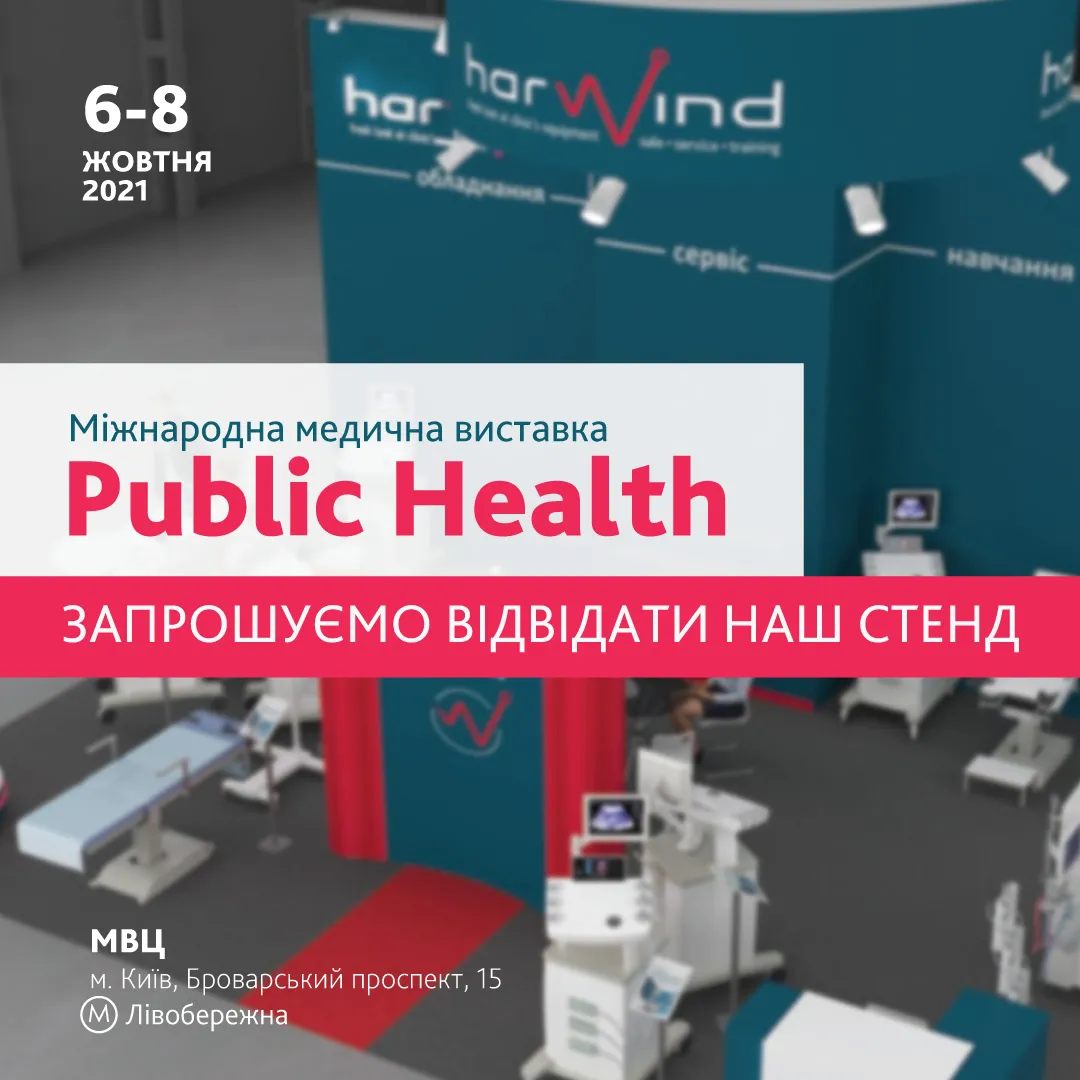
![Article]() Visit the Harwind stand at PUBLIC HEALTH 202122 May 2021We invite you to visit Harwind's stand at PUBLIC HEALTH 2021, which will be held from 6 to 8 October 2021 at the International Exhibition Centre (Kyiv). This is the largest international event in Ukraine and the fourth in Europe. Every year, PUBLIC HEALTH brings together about 300 leading manufacturers and distributors of medical equipment, services, medicines, and medical devices from Ukraine and other countries. For 30 years, the exhibition has been helping to expand the market and strengthen partnerships. This year, our stand will feature diagnostic equipment from world leaders FUJIFILM, Mindray, and SLE. You will be able to get acquainted with stationary and portable ultrasound machines, test a portable ultrasound transducer, and see how artificial intelligence from FUJIFILM works. You will also have the opportunity to get advice from our specialists, learn about the latest equipment and special offers.
Visit the Harwind stand at PUBLIC HEALTH 202122 May 2021We invite you to visit Harwind's stand at PUBLIC HEALTH 2021, which will be held from 6 to 8 October 2021 at the International Exhibition Centre (Kyiv). This is the largest international event in Ukraine and the fourth in Europe. Every year, PUBLIC HEALTH brings together about 300 leading manufacturers and distributors of medical equipment, services, medicines, and medical devices from Ukraine and other countries. For 30 years, the exhibition has been helping to expand the market and strengthen partnerships. This year, our stand will feature diagnostic equipment from world leaders FUJIFILM, Mindray, and SLE. You will be able to get acquainted with stationary and portable ultrasound machines, test a portable ultrasound transducer, and see how artificial intelligence from FUJIFILM works. You will also have the opportunity to get advice from our specialists, learn about the latest equipment and special offers. -
![Article]() A cycle of thematic improvement "Ultrasound examination of patients in the practice of a family doctor" to be held in Kyiv19 August 2022The aim of this course is to train family doctors in the use of ultrasound equipment in their professional activities. Thanks to this, primary care physicians can make more accurate diagnoses at the initial visit
A cycle of thematic improvement "Ultrasound examination of patients in the practice of a family doctor" to be held in Kyiv19 August 2022The aim of this course is to train family doctors in the use of ultrasound equipment in their professional activities. Thanks to this, primary care physicians can make more accurate diagnoses at the initial visit