NMT neuromuscular conductance monitoring method (TOF)
20 July 2023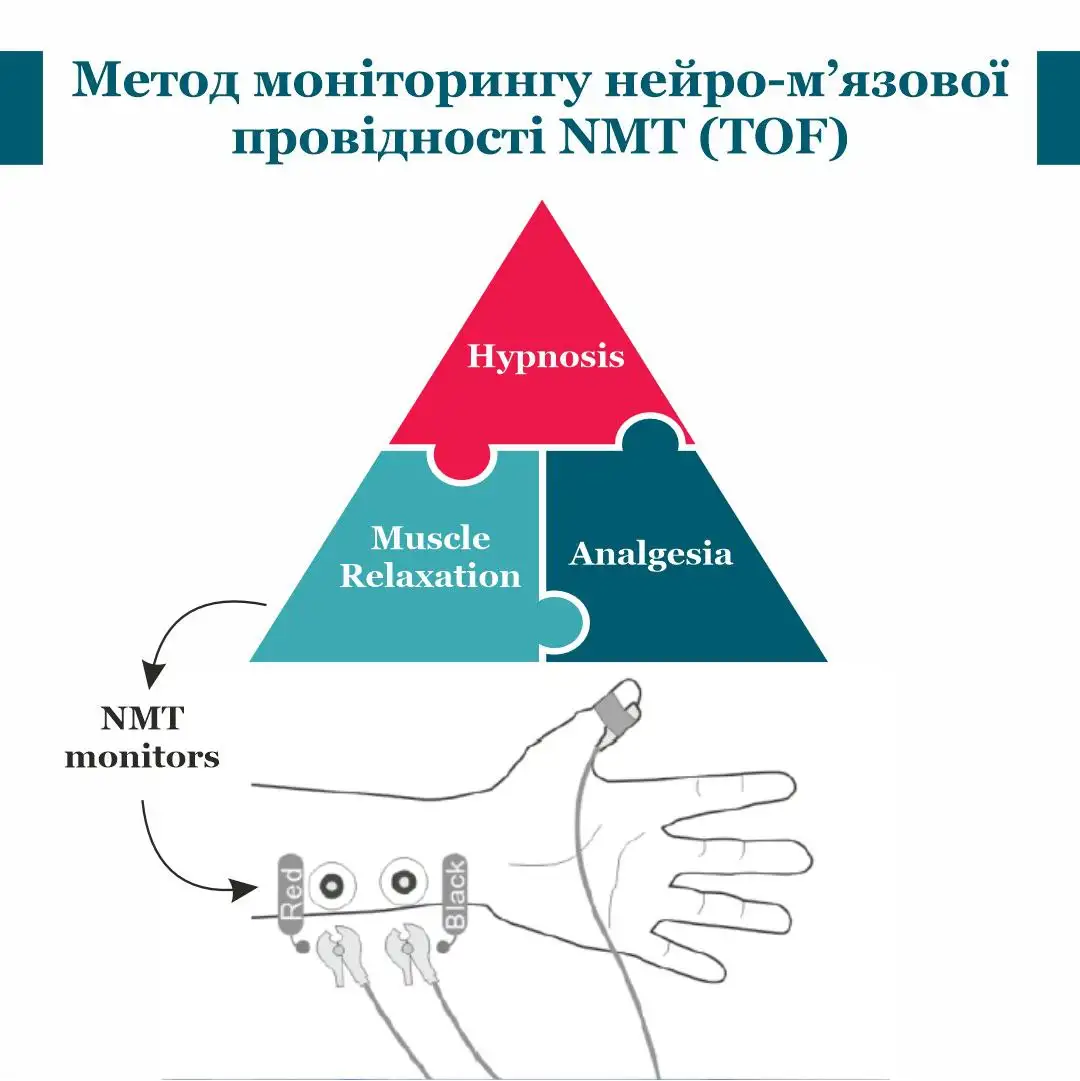
Use
Anaesthetists use muscle relaxants, e.g. for tracheal intubation, maintenance of
anaesthesia and to support the work of surgeons, is almost a daily occurrence. But very
often, we administer muscle relaxants "blindly", calculating a specific dose of mg/kg for
for each individual patient. And patients are different, just like muscle relaxants.
Each patient reacts individually to a particular type of muscle relaxant and the dose
mg/kg is often unreliable [1].
We can observe when, without neuromuscular conduction monitoring, during intubation the patient coughs, raises his arms, etc. Or when, during a surgical procedure surgeons ask the patient to "relax". Or even during extubation the anaesthetist assesses the restoration of neuromuscular conduction using clinical signs (asking to show the tongue, shake hands, tear off the head, etc.). All these clinical signs do not guarantee the exclusion of residual muscle relaxation [2]. А This complication is one of the most dangerous and can lead to desaturation, re-intubation, or even postoperative aspiration pneumonia. pneumonia [3].
With the help of TOF neuromuscular conduction monitoring method, residual muscle relaxation after tracheal extubation can be excluded by 100%. The most authoritative associations of of anaesthetists (Association of British Anaesthetists, European Association of Anaesthetists, American Association of Anaesthetists) indicate in their their guidelines about mandatory Quantitative monitoring of neuromuscular conductance (TOF) in case of use of of muscle relaxants and the exclusion of the possibility of residual muscle relaxation at TOF values before estubation - TOFC 4 TOFR >0.9[4-5].
With the help of TOF can be used to objectively assess the level of neuromuscular blockade during surgical intervention, the level of block depth, which should correspond to a particular surgery. The surgeon's subjective statement during surgery that the patient is not sufficiently "relaxed" can be objectified with this monitoring method and understand whether additional amounts of of muscle relaxant is needed. After all, given that we still do not have widespread use of rocuronium and sugamadex, its antidote, an excessive amount of muscle relaxant at the end of of surgery can lead to residual muscle relaxation after
1. Maybauer DM et al. Anaesthesia 2007;62:12-17
2. Donati:
Can J Anaesthesiology 2013;60:714-29
3. Bulka et
al. Anaesthesiology 2016;125:647-55
4. AA Klein
et al. Anaesthesia 2021;76:1212-1223
5. Fuchs-Buder
T et al. Eur J Anaesthesiol. 2023;40(2):82
6. Thilen SR et al.
Anaesthesiology. 2023;138(1):13
7. Moira H Bruintjes
et al.



